In March 2022, the Queen’s Nursing Institute Scotland conducted an online survey about Fetal Alcohol Spectrum Disorders (FASD). This was a Year 1 activity of Healthier Pregnancies, Better Lives (HPBL) – a QNIS programme supported by Cattanach and The National Lottery Community Fund. All community nurses and midwives anywhere in Scotland were eligible to participate in this survey.

Dr Jonathan Sher

Lisa Lyte

Prof Moira Plant
The introductory blog which you can read here offered a helicopter view of the results of the QNIS/HPBL survey about Fetal Alcohol Spectrum Disorders (FASD). This second blog in the series has a sharper focus and enables the participating community nurses and midwives across Scotland to speak for themselves through their responses.
Despite the pressures, fatigue and other burdens they were confronted with during another spike in COVID-19 cases, 219 of these dedicated, health professionals, in diverse roles all across Scotland, answered our questions and shared their perspectives, knowledge and experience. We thank all who responded for their participation.
The initial four questions were basic demographic ones; the results of which appear in the previous blog. Starting from question 5, let’s examine the responses to the more specific prompts.
Question 5: How comfortable do you feel having a discussion with women of childbearing age about their alcohol consumption and about drinking alcohol in pregnancy?
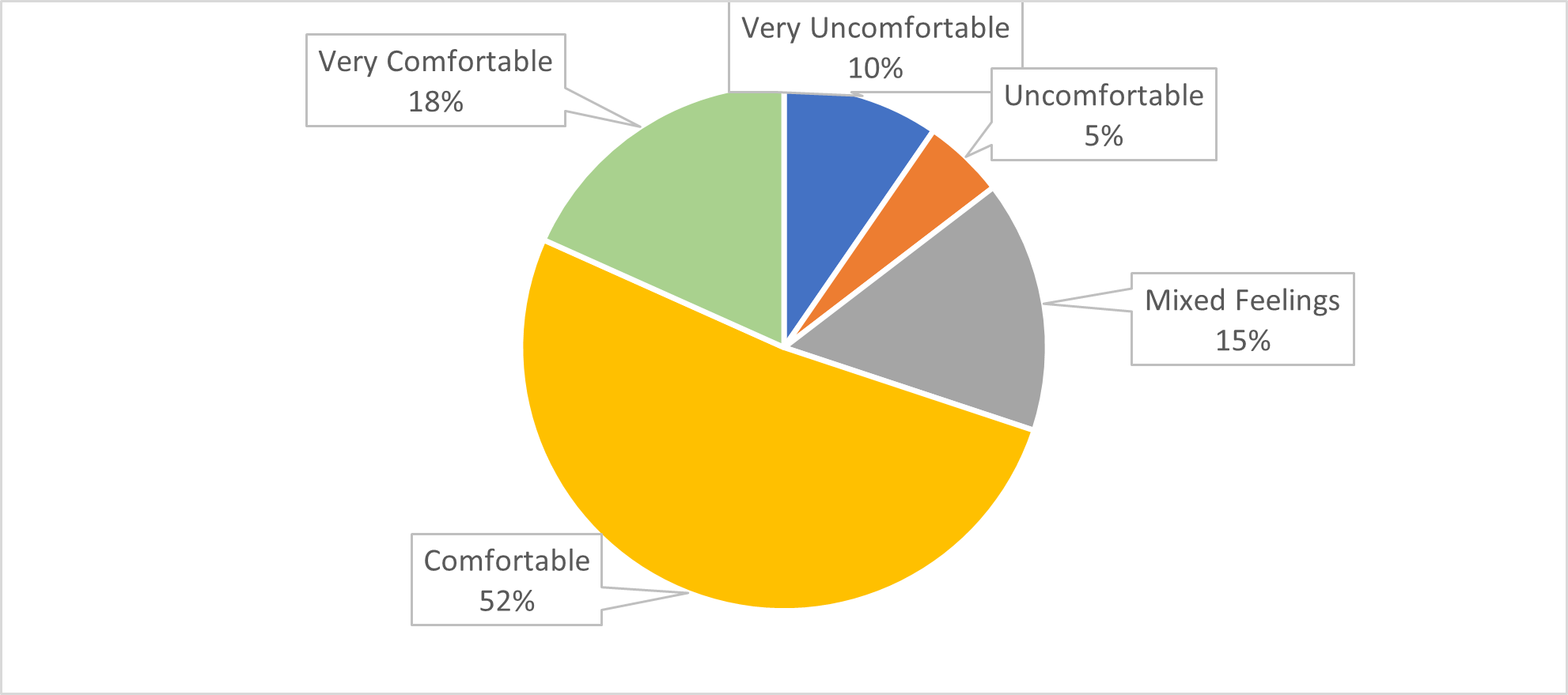 Illustration 1
Illustration 1
Question 6: Do you routinely ask women of childbearing age about smoking tobacco, taking drugs or drinking alcohol?
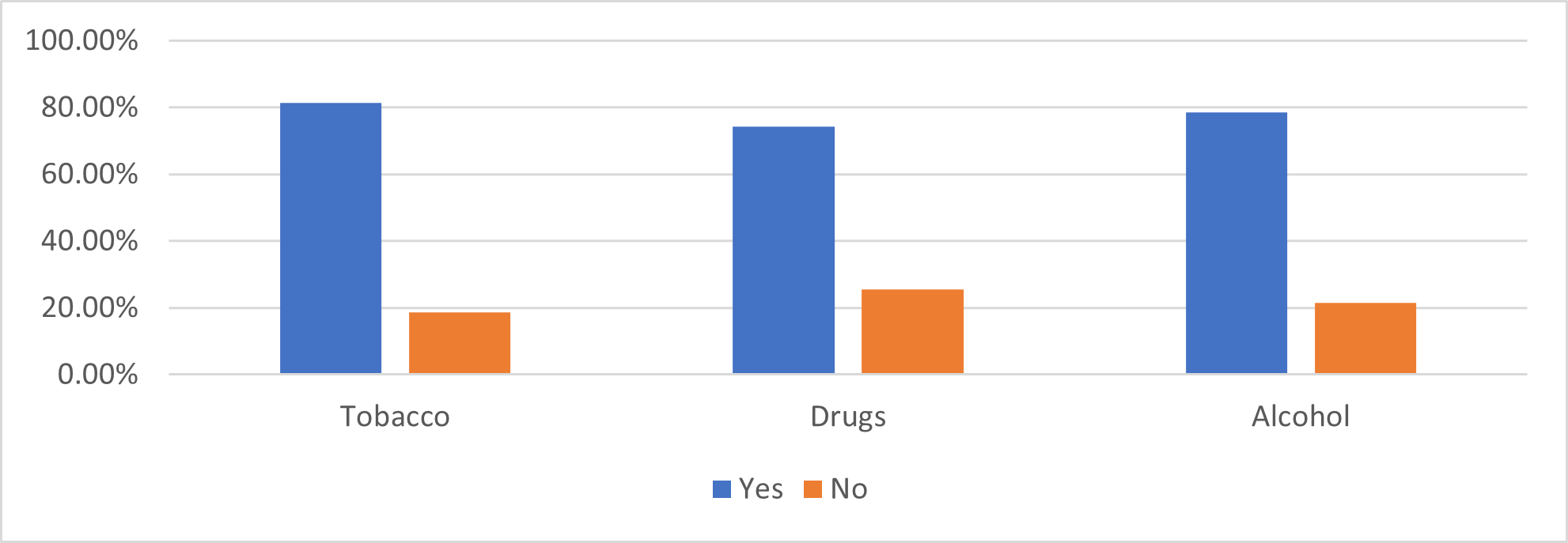 Illustration 2
Illustration 2
On the one hand, it is reassuring that this survey revealed that 80% of the Scottish community nurses and midwives who responded already do discuss alcohol consumption and alcohol-related topics (including drinking during pregnancy) with women of childbearing age (see illustration 2) – and that 70% felt comfortable or very comfortable doing so (see illustration 1).
The reasons most frequently cited were that it was a routine/normal part of their practice and that they had received training to discuss alcohol and/or conduct Alcohol Brief Interventions (ABIs). Drinking was talked about less often than smoking, but more often than taking non-prescription drugs.
On the other hand, it is concerning that approximately 20% of respondents do not usually raise alcohol-related issues with women of childbearing age, and nearly 33% do not feel comfortable discussing this topic. Further survey questions asked about the use of screening tools and the kind of advice or information they shared with these women.
Among those who do explore alcohol consumption, fewer than half use any standard screening tools, while 88% have conversations about drinking, smoking and non-prescription drug-taking ‘in a more general way’. This is not a criticism. In part, it reflects the fact that many community nurses and midwives are skilled at eliciting the information needed through such conversations.
But we cannot assume this as universal knowledge. Developing stronger listening skills is vital and too often overlooked in the initial education and continuing professional development of community nurses and midwives. Given these survey results, it is clear these committed professionals want to offer the best care. Enhancing listening skills and receiving updated information on risks and interventions would greatly increase both their proficiency as well as their confidence to have conversations about drinking in helpful ways. Discussions about alcohol consumption before, during and after pregnancy do not happen in a vacuum. Placing pregnancy in the context of people’s alcohol-related realities and hopes is the key.
When giving advice about drinking alcohol during pregnancy, most of these community nurses and midwives echoed the Scottish Government’s ‘no alcohol, no risk’ message, advocating no alcohol at any time while pregnant. However, a significant minority indicated they instead encourage nothing more than cutting down on drinking, especially during the first trimester.
The following quotes reflect their wide-ranging comments, perspectives and experiences:
 The overall impression emerging from this part of the survey is one of individuality and heterogeneity. Some respondents are clearly comfortable, competent and confident to ask questions, initiate conversations and offer information, advice and signposting on alcohol issues. Others are equally clearly neither prepared nor keen, to address drinking among their patients/clients of reproductive age.
The overall impression emerging from this part of the survey is one of individuality and heterogeneity. Some respondents are clearly comfortable, competent and confident to ask questions, initiate conversations and offer information, advice and signposting on alcohol issues. Others are equally clearly neither prepared nor keen, to address drinking among their patients/clients of reproductive age.
There is a broad recognition that Scotland has an ‘unhealthy relationship with alcohol’. Similarly, it is not a secret among the respondents that alcohol and pregnancy don’t mix (at least not well). Yet, the heterogeneity observed speaks more to the longstanding societal ‘blind spot’ in relation to FASD – and its absence from their initial education and CPD – than to any personal or professional shortcomings of these practitioners. Like the women in their practices, community nurses and midwives do not deserve to be named, blamed or shamed for the outsized role alcohol plays in our society, economy, culture and personal lives.
Moving ever closer to a healthier relationship with alcohol should be everyone’s goal. Community nurses and midwives have a responsibility and unique opportunity, as trusted, respected, community-based health professionals, to take the next step.
This happens by refining their knowledge and ability to make connections between alcohol consumption and pregnancy/birth outcomes. Recognising and understanding FASD offers a compelling new reason to engage people in meaningful, non-judgmental, fact-based, compassionate and person-centred conversations about the role of alcohol in their lives, health and wellbeing.
This is the second blog in a series of four, you can read the other blogs here: